Diabetic Retinopathy
What is Diabetic Retinopathy?
At the Jacksonville Eye Center, Dr. Schnipper and the rest of his wonderful staff make it their number one priority to improve the sight of every single patient who walks into our doors. Diabetic Retinopathy is a common eye disease that can be treated right in our office.
Diabetic retinopathy is the most common diabetic eye disease and a leading cause of blindness in American adults. In the majority of diabetic retinopathy cases, blindness is completely preventable. Patients will need to work closely with Dr. Schnipper to monitor and treat this disease. The use of medications and daily blood sugar monitoring can make a major impact on containing the worsening of diabetic retinopathy. The retina is like the film in a camera; in which it is the light-sensing film on the back of the eye that captures the images.

Diabetic Eye Disease
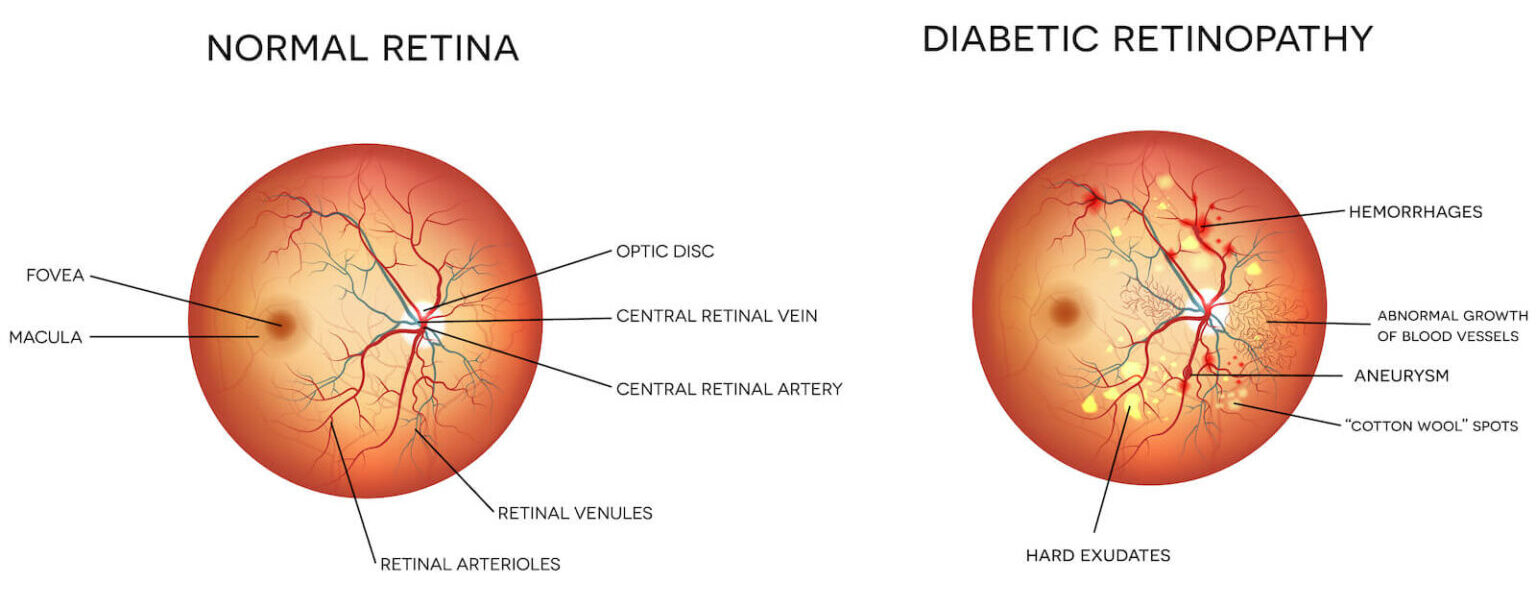
In the diabetes disease, sugar (glucose) builds up within blood vessels in the retina and tissues of the body causing it to attach to the proteins in the wall. This alters the vessel’s normal structure and functioning. The vessels eventually get blocked and leak fluid. When they cannot deliver an adequate amount of blood supply to the eye, the eye can generate abnormal new blood vessels. Early diabetic retinopathy usually has no symptoms. However, worsening diabetic retinopathy can lead to visual loss and blindness.
Causes of Diabetic Retinopathy
Diabetic retinopathy develops when high blood sugar levels damage the small blood vessels in the eye. there are two types of diabetic retinopathy, nonproliferative and proliferative. Each has slightly different characteristics but both relate to uncontrolled blood sugar.
Nonproliferative diabetic retinopathy involves microaneurysms, retinal swelling, “cotton wool spots”, and retinal hemorrhages. Proliferative diabetic retinopathy is more advanced, involving neovascularization and the growth of new blood vessels that permeate the back and front of the eye over time. These new blood vessels are weak and can bleed, causing scar tissue to form on the retina. The vessels can also obstruct drainage from the eye, leading to increased intraocular pressure.
Who is at Risk for Developing Diabetic Retinopathy?
This eye disease is a complication experienced by diabetics. However, it isn’t as simple as this. Studies suggest that the risk of diabetic retinopathy is influenced by several factors, including:
Duration of Diabetes
It has been estimated that approximately 90% of people with Type 1 diabetes for longer than 10 years will develop some degree of retinopathy. The estimate is approximately 67% for Type 2 diabetics who do not take insulin. Furthermore, approximately 79% of ten-year Type 2 diabetics who do take insulin may develop retinopathy. Gestational diabetes also presents a risk of retinopathy.
Blood Sugar
The higher blood sugar levels are on a consistent basis, the greater the chance a person will develop diabetic retinopathy.
Smoking
Like diabetes, smoking damages blood vessels throughout the body, including the small vessels in the eye. When a diabetic is also a smoker, the risk of retinopathy increases substantially.
High Blood Pressure
The combination of high blood sugar and high blood pressure exponentially increases the risk of retinopathy due to the ways blood vessels are affected by each of these conditions.
Diabetic Retinopathy Symptoms
Diabetic retinopathy does not really have any initial warning signs. Dr. Schnipper suggests that all diabetic patients have regular eye examinations to monitor your eyes for changes.
If proliferative diabetic retinopathy is left untreated blindness can occur. The best alternative to fighting PDR is early detection. It is important for diabetics to have regular eye exams to watch for PDR.
Is Diabetic Retinopathy A Common Disorder?
Diabetic retinopathy is the most common cause of visual impairment and vision loss among American adults. The Centers for Disease Control and Prevention estimates that cases of diabetic retinopathy will nearly double by 2050, affecting approximately 14.6 million people in the next thirty years.
Patient Testimonials
Diagnosing Diabetic Retinopathy
The diagnosis of diabetic retinopathy requires a thorough eye exam in order to be accurate. Prior to these tests, we will administer a stain eye drop in order to see the blood vessels more clearly. The eye examination includes the following:
Early detection of diabetic eye disease is the best way to ensure that you receive the proper treatment. If you are concerned you may be afflicted with diabetic retinopathy, consider scheduling a consultation at Jacksonville Eye Center today.

What Are The Stages of Diabetic Retinopathy?
The stages of diabetic retinopathy are divided into two categories, nonproliferative retinopathy, and proliferative retinopathy.
Nonproliferative Retinopathy
This is the first and earliest stage of diabetic retinopathy. NPDR occurs when the small blood vessels of the retina start to leak fluid or bleed. This activity will lead to the formation of deposits called exudates. Once these blood vessels start to leak swelling within the central part of the retina occurs. When the leakage of these blood vessels causes swelling, macular edema sets in and the blood vessels can become blocked. This stage of diabetic retinopathy is common when a person develops diabetes. Most diabetics have some grade of NPDR. It is imperative to maintain regular eye examinations with the retina specialists at Inland Eye Specialists to monitor and treat NPDR.
Proliferative Retinopathy
When new vessels start to grow as a result of the existing vessels becoming blocked, this marks the beginning of the next stage of diabetic retinopathy, proliferative diabetic retinopathy. This level of diabetic retinopathy is the most severe and dangerous for diabetic patients. These new abnormal blood vessels can grow on the retina, optic nerve, iris or into the vitreous gel inside the eye, and tend to grow poorly and are very fragile. The damage that these blood vessels bring to the retina can be catastrophic and include hemorrhages on the retina, scar tissue build-up, and possible retinal detachment.
Diabetic Retinopathy Treatment Options
For the first three stages of Diabetic Retinopathy, the most important treatment for you is controlling your blood sugar, cholesterol, and blood pressure. Unfortunately, if stage four occurs, laser surgery known as scatter laser treatment will be needed. The procedure is when abnormal blood vessels become ablated, meaning they begin to shrink. It works best when the blood vessels in your eyes start bleeding. If it becomes severe, it will be corrected with what is called a vitrectomy. All blood will then be removed from the eye.
Diabetic Retinopathy FAQ
Schedule a Consultation
For more information about Diabetic Retinopathy and treatment options, contact Jacksonville Eye Center at 904-355-5555 to schedule a consultation.